Introduction
Cataract surgery has come a long way since its inception, with significant advancements transforming it into a minimally invasive procedure that promises improved outcomes and faster recovery. One of the most notable innovations in cataract surgery is microincision cataract surgery, a technique that has revolutionized the field by allowing surgeons to perform cataract removal through smaller incisions. This article delves into the intricacies of microincision cataract surgery, its benefits, techniques, and the impact it has had on patient care and ophthalmology as a whole.
Understanding Cataracts
Cataracts, the clouding of the eye's natural lens, are a common cause of vision impairment, particularly in older individuals. As cataracts progress, they can lead to blurry vision, reduced color perception, and increased sensitivity to light. Traditional treatment involves surgically removing the cloudy lens and replacing it with an intraocular lens (IOL) to restore vision.
Evolution of Cataract Surgery
Historically, cataract surgery involved larger incisions, often resulting in lengthy recovery times and potential complications. Over the years, surgeons have refined their techniques and instruments, leading to the development of phacoemulsification – a procedure that uses ultrasonic energy to break up and remove the cloudy lens through a small incision. This innovation marked a significant leap forward, allowing for faster healing and reduced surgical trauma.
Enter Microincision Cataract Surgery
Microincision cataract surgery takes the principles of phacoemulsification a step further by utilizing even smaller incisions, typically around 1.5 to 2.0 millimeters in size. This advancement is made possible by the development of specialized instruments and techniques that enable surgeons to perform precise maneuvers within the eye with minimal trauma.
Techniques and Tools
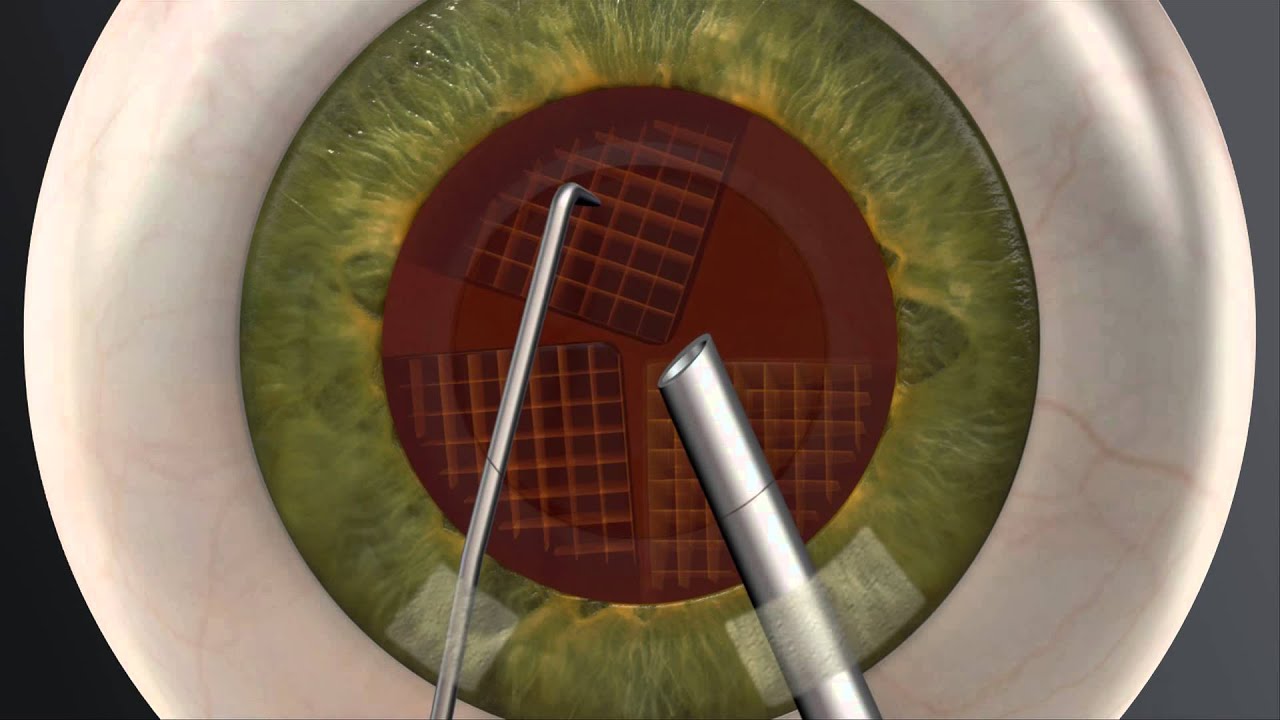
Several techniques fall under the umbrella of microincision cataract surgery, each with its own nuances and advantages. Some commonly employed techniques include:
Bimanual Microincision Cataract Surgery (B-MICS): In this technique, two separate instruments are used – one for holding the eye steady and the other for performing the surgical maneuvers. This approach provides enhanced control and flexibility, enabling delicate procedures with minimal tissue disruption.
Microcoaxial Cataract Surgery: Here, a single instrument serves both irrigation and aspiration functions, reducing the need for multiple instrument exchanges. This streamlined process minimizes fluid turbulence within the eye and enhances surgical efficiency.
Femtosecond Laser-Assisted Microincision Cataract Surgery: This technique combines the precision of femtosecond laser technology with microincision surgery. The laser assists in creating corneal incisions and softening the cataract, potentially reducing the energy needed during phacoemulsification.
Benefits and Advantages
Microincision cataract surgery offers a multitude of benefits for both patients and surgeons:
Faster Recovery: Smaller incisions lead to reduced surgical trauma, resulting in quicker healing times and enhanced patient comfort.
Minimal Astigmatism: Microincisions are strategically placed to reduce induced astigmatism, leading to improved postoperative vision quality.
Reduced Risk of Infection: Smaller wounds have a lower risk of infection, contributing to better surgical outcomes.
Less Induced Inflammation: Microincision surgery causes less disruption to ocular tissues, resulting in fewer inflammatory responses.
Preservation of Corneal Architecture: The smaller incisions help maintain the structural integrity of the cornea, leading to better long-term visual outcomes.
Challenges and Considerations
While microincision cataract surgery boasts numerous advantages, it's important to acknowledge certain challenges:
Skill Requirement: Surgeons need specialized training to master the intricacies of microincision techniques due to the precision and dexterity required.
Equipment Costs: The instruments and equipment for microincision surgery can be costlier than traditional instruments.
Patient Suitability: Not all patients are suitable candidates for microincision surgery, and individual anatomical factors must be considered.
Conclusion
Microincision cataract surgery represents a paradigm shift in the field of ophthalmology, offering patients the promise of improved visual outcomes and quicker recovery times. This innovative technique, driven by advancements in instrumentation and surgical approaches, has redefined cataract surgery as we know it. As technology continues to evolve, microincision cataract surgery is likely to become even more refined, ensuring that patients around the world receive optimal care for their vision-related needs.